 Bedsores (also referred to as pressure injuries or decubitus ulcers) are lesions that are caused when unrelieved pressure damages underlying tissues on bony surfaces, such as the tailbone, hip, heel, back, and back of the head. Bedsores often arise when nursing home residents lie for long periods of time in a single position. Therefore, prevention generally consists of repositioning residents frequently, so they are not sitting or lying in one position for extended periods and using specialty cushions to help minimize the risk of developing these painful lesions. Additionally, the skin must be kept clean and dry, and proper nutrition and hydration are essential.
Bedsores (also referred to as pressure injuries or decubitus ulcers) are lesions that are caused when unrelieved pressure damages underlying tissues on bony surfaces, such as the tailbone, hip, heel, back, and back of the head. Bedsores often arise when nursing home residents lie for long periods of time in a single position. Therefore, prevention generally consists of repositioning residents frequently, so they are not sitting or lying in one position for extended periods and using specialty cushions to help minimize the risk of developing these painful lesions. Additionally, the skin must be kept clean and dry, and proper nutrition and hydration are essential.
 Federal law mandates that nursing homes conduct regular assessments of patients to determine their risk of developing painful pressure sores. Unfortunately, nursing homes and assisted care facilities often fail to conduct mandatory assessments and implement personalized care plans, resulting in countless elderly residents developing painful ulcers, infections, and other potentially life-threatening injuries.
Federal law mandates that nursing homes conduct regular assessments of patients to determine their risk of developing painful pressure sores. Unfortunately, nursing homes and assisted care facilities often fail to conduct mandatory assessments and implement personalized care plans, resulting in countless elderly residents developing painful ulcers, infections, and other potentially life-threatening injuries.
If you, your parent, or a loved one developed a bedsore while living in a nursing home or assisted-living facility, we invite you to call our office to schedule a free consultation to learn about your legal options for seeking accountability and maximum compensation for your injuries and damages.
What are Bedsores?
According to the Mayo Clinic, pressure sores are injuries to the skin and underlying tissues resulting from extended pressure on the skin.[1] Bedsores most often develop on tissue covering bony areas, such as the:
 Tailbone
Tailbone- Buttocks
- Shoulder blades
- Spine
- Back of arms or legs (where they rest against a chair)
- Back or sides of the head
- Heels, ankles, and skin behind the knees
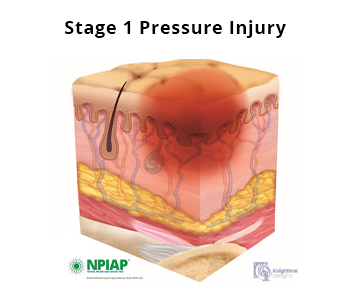
Individuals with mobility issues or who spend most of their time in a bed or chair are most at risk for the development of pressure ulcers. Bedsores typically develop in the following four stages:
 Stage 1. The skin may experience changes in color (redness), warmth, or consistency.
Stage 1. The skin may experience changes in color (redness), warmth, or consistency.
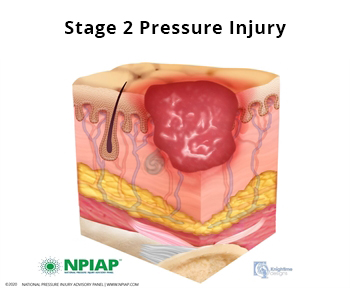
- Stage 2. The top two layers of skin break open.
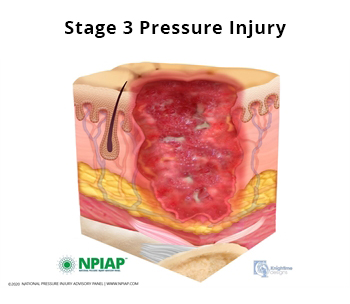
- Stage 3. The sore has broken through the first two layers of skin and into the fatty tissue.
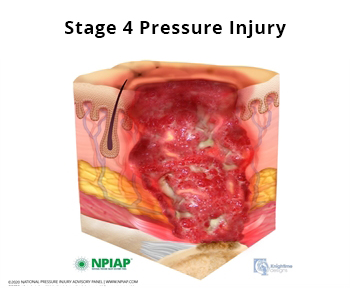
- Stage 4. Skin and tissue loss with exposure of muscle or bone.
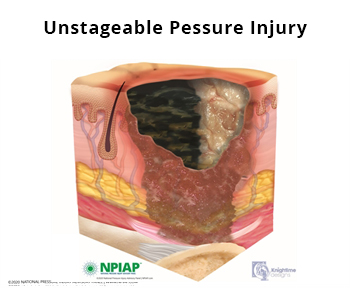
- Unstageable. The underlying tissue is obscured by slough or eschar.
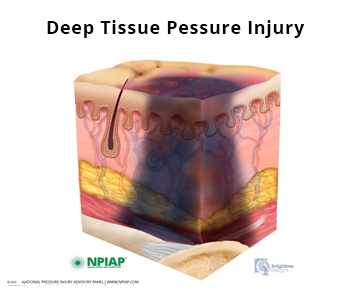
- Deep Tissue Pressure Injury. Deep color changes with a dark wound bed, resulting from intense and/or prolonged pressure and shear forces at the bone-muscle interface.[2]
Bedsores falling within Stages 1 and 2 may heal within a few weeks or months. However, Stage 3 or 4 ulcers can require significant surgical intervention to remove dead tissue. With advanced bedsores (i.e., Stages 3 and 4, unstageable, and deep tissue pressure injuries), there is also a risk of life-threatening infection.
How Are Bedsores Treated?
Care for bedsores typically requires immediate medical intervention and a team approach, with nursing staff working closely with physicians and wound care specialists. Without proper care, a pressure ulcer can rapidly develop into a larger, infected ulcer.
 Nursing homes are required by federal law to perform assessments to identify a resident’s specific risk factors. Then, the care team must create a personalized plan of care to reduce the risk of developing such conditions. For example, if an individual is at high risk for developing pressure ulcers, his or her plan of care should involve turning and repositioning the individual at least every two hours, keeping the skin clean and dry, and ensuring that proper nutrition and hydration are provided.
Nursing homes are required by federal law to perform assessments to identify a resident’s specific risk factors. Then, the care team must create a personalized plan of care to reduce the risk of developing such conditions. For example, if an individual is at high risk for developing pressure ulcers, his or her plan of care should involve turning and repositioning the individual at least every two hours, keeping the skin clean and dry, and ensuring that proper nutrition and hydration are provided.
Are Nursing Homes Liable If a Patient Develops Bedsores?
Federal laws govern the care provided to residents by nursing homes, including regulations specific to bedsores. The regulations state that a
nursing home must provide care to prevent pressure ulcers and ensure that a resident does not develop pressure ulcers, and must provide necessary treatment and services to promote healing, prevent infection and prevent new ulcers from developing.[3]
A bedsore is avoidable when the nursing home does not do one or more of the following:
 Evaluate the resident’s clinical condition and risk factors;
Evaluate the resident’s clinical condition and risk factors;- Define and implement interventions that are consistent with resident needs, resident goals, and professional standards of practice;
- Monitor and evaluate the impact of the interventions; or
- Revise the interventions as appropriate. [4]
Individuals entering nursing homes without pressure ulcers should not develop bedsores unless it is “medically unavoidable.”
Medically unavoidable means that a resident developed a bedsore even though the nursing home:
- Performed an accurate and complete assessment;
- Developed a care plan which is implemented consistently and based on data from the assessment; and
- Evaluated the results of the interventions and revised the interventions as necessary.[5]
When nursing homes, long-term care facilities, and assisted living facilities fail to follow federal or state regulations and their own internal policies in both assessing a patient’s risk factors and implementing a personalized care plan, the care facility (and its insurer) may be liable for damages attributable to the injuries, including monetary compensation for:
- Medical expenses
- Pain and suffering
How Much Does A Michigan Nursing Home Bed Sore Lawyer Cost?
As experienced nursing home bedsore attorneys, we understand how devastating it can be when a parent or loved one suffers injuries while in the care of a nursing home or assisted living facility. As such, the last thing we believe you should have to worry about is coming out of pocket for legal representation. For this reason, we represent nursing home abuse victims and their families on a contingency-fee basis, meaning we are only entitled to a fee if compensation is secured.
If you or a loved one developed pressure ulcers while in the care of a nursing home or assisted living facility, we invite you to call our office today to schedule a free consultation with an experienced nursing home bedsore lawyer. We can listen to the facts of your case and explain your legal options for seeking justice, accountability, and the maximum compensation to which you and your loved ones are rightfully entitled.
[1] Bedsores (pressure ulcers), Mayo Clinic, Bedsores (pressure ulcers) – Symptoms and causes – Mayo Clinic.
[2] National Pressure Injury Advisory Panel Pressure Injury Stages, https://npiap.com/page/PressureInjuryStages.
[3] 42 USC 483.25(b).
[4] CMS Manual, Centers for Medicare and Medicaid, https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R22SOMA.pdf.
[5] Id.
